Mostrar Contenidos Sensibles

Download pdf (268k)
The introduction of oncoplastic techniques in the conservative management of breast cancer has improved the quality of cosmetic results, especially in areas at high risk of deformity, such as the lower pole and inner quadrants. It has allowed breast conservation in women with multifocal/multicentric tumours and has enabled breast irradiation in women with macromastia. However, conservative management of the breast is problematic in cases where there is a wide dispersion of disease (multifocality, multicentricity), or where the initial lesions persist after neoadjuvant therapy (extensive microcalcifications). In this context, mastectomy is the best approach for this patient subset.
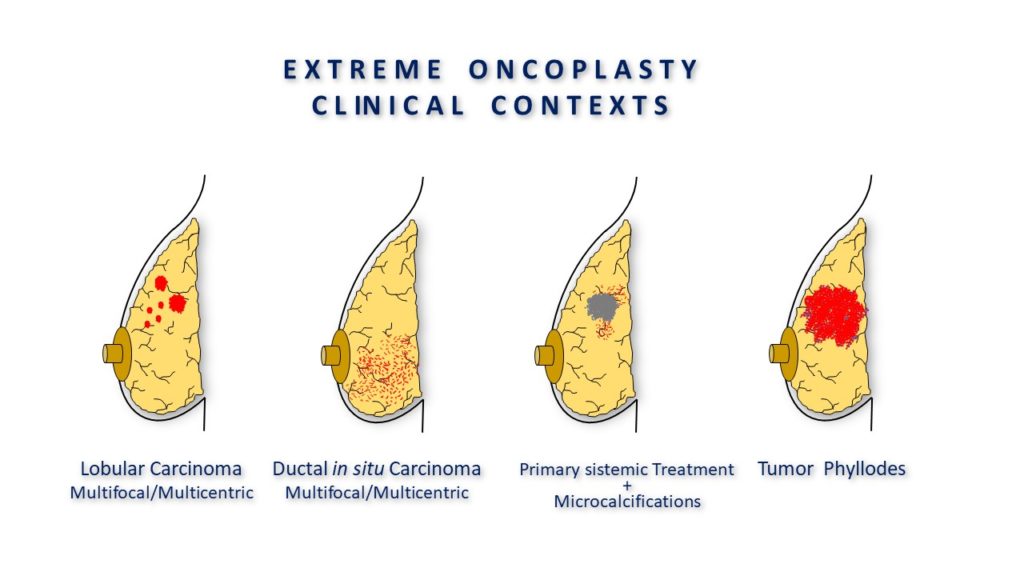
The term "extreme" oncoplastic surgery (eOBCS) was defined by Silverstein as a breast conserving procedure which, through the use of oncoplastic techniques, is offered to a patient who would normally require a mastectomy according to the majority of surgeons. This applies to women with tumours greater than 5 cm (many of which are multifocal or multicentric), ductal carcinomas in situ greater than 5 cm, or locally advanced tumours with a partial response to neoadjuvant chemotherapy, as well as previously irradiated patients. In these situations, the oncoplastic procedure offers women a final opportunity for breast conservation before resorting to mastectomy, which, in most cases, will require postoperative radiotherapy. However, there is a lack of information about the safety of these procedures as, with the exception of a series published by Silverstein, most studies only present isolated cases of extreme breast conservation. As a result, the impact of extreme oncoplasty on global and disease-free survival, patient satisfaction, and quality of life in patients who have undergone such a procedure is unknown.
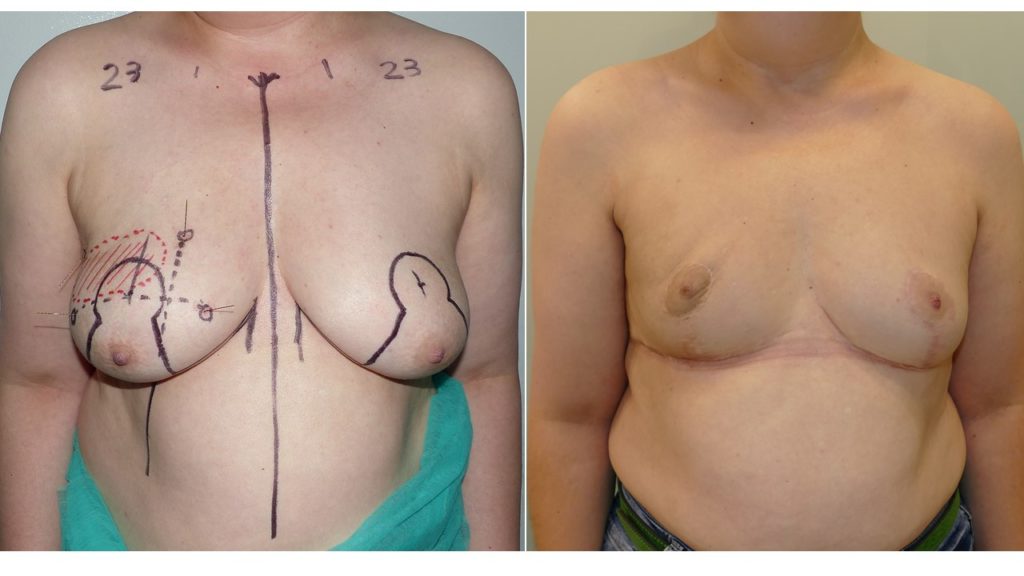
Our Experience
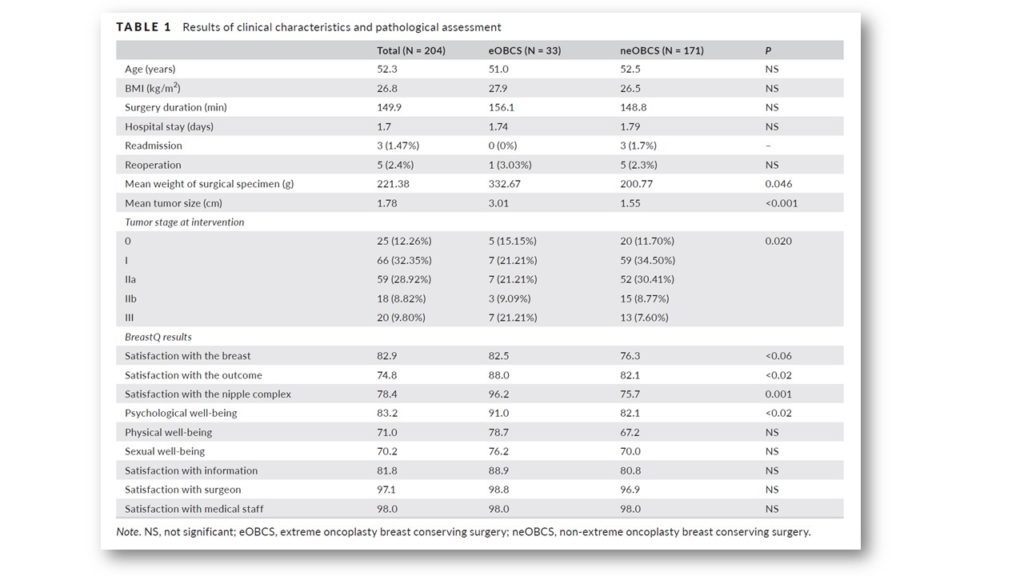
A total of 1,198 patients underwent surgery during the study period, of which 204 met the inclusion criteria. The case group was made up of 33 eOBCS patients. eOBCS was indicated in patients with larger tumours and those with greater tumour dispersion. The mean weight of the surgical specimen was significantly greater in the eOBCS, as was the mean tumour size, with a greater presence of T3 tumours. The incidence of bleeding and tissue/nipple-areolar complex necrosis during the postoperative period was low in both groups. Re-excision of margins was necessary in 12.5% of eOBCS patients and in 8.1% of neOBCS patients, with a low incidence of mastectomy (3.1% in eOBCS and 1.1% in neOBCS).
The mean patient follow-up was 66.6 ± 45.5 months. During this time, 21 locoregional recurrences were diagnosed, suggesting a 10-year actuarial incidence of 9.0% and 9.1% for the eOBCS and neOBCS groups, respectively. Actuarial survival at 10 years was 88%.

Women that underwent eOBCS reported significantly greater satisfaction with the breast, evolution, their psychosocial well-being and the condition of the nipple (Table 2). In addition, they achieved a nominally higher score for sexual and physical well-being, as well as satisfaction with the informative process.
Oncoplastic surgery has proven to be a good alternative to lumpectomy for the conservative management of breast cancer, facilitating oncological resection and improving quality of life for the affected women. In terms of oncological safety, overall and disease-free survival are the key outcomes of interest when evaluating oncoplastic surgery, lumpectomy and mastectomy. Early studies comparing lumpectomy to mastectomy showed a similar overall survival, though a higher rate of local recurrences with breast conservation. The incidence of local failure at 10 years ranged from 8.8% in the Milan Trial to 19% in the EORTC study. Since then, several authors (12-23) have published their experience in the use of oncoplastic techniques for the treatment of breast cancer; however, most of these studies have a very short mean follow-up (ranging from 1.5–3.8 years), and do not present an actuarial analysis of overall or disease-free survival.
Only three studies have analysed survival and the incidence of local relapse after oncoplastic surgery with follow-up periods of 5 and 10 years. Clough et al. analysed the safety of oncoplastic procedures in 350 patients, with no limit of tumour size (T1, T2 and T3) or lymph node involvement (N0, N1), and found the incidence of local relapse at 5 years to be 2.2%. Describing the experience of the Milan European Institute of Oncology, Lorenzi et al. reported the incidence of local relapse to be 6.7% at 10 years. Finally, Acea et al. analysed the evolution of 170 women undergoing oncoplastic breast reduction and found a local relapse incidence of 4.7% and 9.8% at 5 and 10 years, respectively. In these three studies, no difference in overall survival were observed between lumpectomy and oncoplastic procedures. These experiences confirm two ideas in patients undergoing oncoplastic procedures. Firstly, the current overall survival of patients subjected to oncoplastic procedures (84–91% at 10 years) is higher than that recorded 30 years ago in clinical trials validating conservative surgery (58–66% at 10 years). This is thanks to the use of systemic treatment in all patients, the use of antibodies in patients with HER2 and specific systemic treatment according to tumour biology. Secondly, there is a lower incidence of local relapse in patients undergoing oncoplastic procedures (6.7–9.8% at 10 years) compared to that recorded in early clinical trials (10.0–19.7% at 10 years). This is despite breast conservation now being indicated in patients with tumours of greater size and greater dispersion (excluded in the B06, Milan and EORTC studies) and tumours with greater lymph node involvement (excluded in the Milan study), as well as a more liberal definition of tumour-free margin ("no tumour in the ink" vs. 1-2 CMS of safety margin). These two facts are a consequence of progress in the locoregional and systemic treatment of breast cancer, which has led to a lower rate of local relapse and an increase in overall survival after conservative surgery, benefits also applicable to oncoplastic surgery.



Conversely, the oncological safety of eOBCS has not been analysed previously, since most studies are clinical cases or series without actuarial analysis of overall or disease-free survival. The series published by Silverstein in 245 patients treated using an eOBCS procedure showed a local relapse incidence of 1.5% at a mean follow-up of 24 months, but did not provide actuarial data at 5 and 10 years. To our knowledge, the present study constitutes the only eOBCS experience to provide data regarding its impact on the survival and quality of life of women with breast cancer. The study demonstrates an oncologic control similar to that of neOBCS over a mean follow-up of 65.6 months. The incidence of local relapse at 10 years in patients with eOBCS procedures (12.5%) was similar to that for patients undergoing neOBCS procedures (9.9%). This difference was not significant, despite the fact that tumours of larger size, greater dispersion and at more advanced stages were included in the case group. Conversely, this study shows greater difficulty in obtaining tumour-free margins in patients undergoing eOBCS, which significantly increases the need for re-intervention to expand margins (12.5% vs. 8.1%). This may be due to the greater spread of disease in this group. However, it did not significantly increase the indication for mastectomy (3.1% vs. 1.1%); thus, breast preservation was achieved in most eOBCS patients. In light of our data, we believe that use of oncoplastic breast reduction allows women with large and widely dispersed tumours to opt for extreme conservation of their breast, with a low likelihood of mastectomy, an overall survival similar to other patients with tumours of a similar stage and biology, and an incidence of local relapse similar to that of patients undergoing other oncoplastic procedures. In our opinion, oncoplastic breast reduction is the ideal oncoplastic approach to breast resection under extreme conditions, as it allows a wide resection of the affected area, facilitates remodelling of the remaining tissue to construct a new breast, and permits breast conservation in almost all patients.
Breast reduction oncoplasty improves cosmetic outcomes as it prevents deformities in the mammary contour and guarantees symmetry under better conditions than those provided by lumpectomy. Studies by Veiga and Hart have demonstrated an improvement in quality of life and self-esteem in women undergoing oncoplastic procedures compared to those undergoing lumpectomy. A study by Losken identified an improvement in the emotional state, breast satisfaction and feeling of attractiveness in recipients of a reductive oncoplasty. In our study, analysis of patient satisfaction and quality of life showed that the eOBCS group reported higher values for all items compared to the neOBCS group. This improvement is especially striking in terms of satisfaction with the nipple (96 vs. 75), perhaps because this anatomical element constitutes the maximum expression of breast conservation. It also highlights the greater satisfaction of eOBCS patients with the information that they received (88.9), which without doubt reflects the surgeon's endeavour to highlight the limitations of breast conserving techniques during the informative process, along with their consequences. In our opinion, patients that have undergone eOBCS are more satisfied as they have understood the potential reality of mastectomy during the informative process and therefore particularly value the result of their breast conservation.
In conclusion, eOBCS for oncoplastic breast reduction allows a high rate of breast conservation, with 10-year overall survival and local relapse rates that are similar to those seen with neOBCS. Patients that undergo eOBCS have a significantly greater satisfaction and quality of life than those that undergo neOBCS.