Mostrar Contenidos Sensibles
The Breast Journal has published the preliminary results of our study in which we evaluated the quality of life in women with oncoplastic breast reduction (OBR) and its predictive factors.
Download archive (383Kb)
This study identified women with macromastia as the group that most benefited from OBR in terms of satisfaction, physical wellbeing and sexual wellbeing. The data confirm that systemic treatments affect satisfaction with the breasts and physical wellbeing. Lastly, the study identified women with a high assessment of their breasts at diagnosis as the group who most likely would be less satisfied with their breasts postsurgery.
Patients and Method
We conducted a prospective study between October 2014 and June 2019 on women with a histological diagnosis of infiltrating carcinoma or ductal carcinoma in situ who underwent OBR in our breast unit. We excluded from the study those patients whose breasts were irradiated prior to the surgery, those who did not undergo symmetrization, those with local or systemic progression of the disease during the study, those who did not undergo radiation therapy adjuvant to the surgery and those who declined to participate in the study.
Study of satisfaction and quality of life. The patients were informed of the disease diagnosis during the first visit in the doctor's office. Simultaneously, the surgical options specific to their breast and tumor were assessed. The unit’s tumor committee subsequently assessed each patient individually and proposed a surgical recommendation. In those cases in which OBR was recommended, the patient was informed of this proposal during the second consultation. During this visit, the patients were informed of the study’s details and asked to participate. Patients who agreed to participate were asked for their authorization through an informed consent document specific for this study and were given the preoperative module of the Breast-Q™ questionnaire (preoperative module on reduction/mastopexy) to determine their satisfaction and quality of life prior to the surgery. The members of the breast unit gave the patients the postoperative module 12 to 24 months after the patients had completed the radiation therapy. The final score for each module was calculated according to the Mapi Research Trust criteria (10) and ranged from 0 to 100 (the higher the score, the greater the satisfaction). For the patients included in the study, we analyzed the following clinical and oncologic characteristics: age, body mass index (BMI), comorbidities, smoking, hormonal state, tumor characteristics, TNM anatomical stage, postoperative complications, radiation therapy and systemic therapies (hormone therapy, chemotherapy, monoclonal antibodies), as well as data regarding their assessment of satisfaction and quality of life before and after the surgery. Currently, the patient inclusion period for the BreastQ-15 study remains open; a second assessment at 5 years of the breast irradiation will be conducted.
The study was evaluated and authorized by the research ethics committee of Galicia, Spain (code, BreastQ-15 2015/571).
Surgical technique. OBR was indicated for the women with multifocal tumors that required broad breast resection, tumors located in areas at risk for deformity (lower pole, upper inner quadrant) and for patients with macromastia. OBR consisted in a Wise pattern, and the pedicle selection was performed according to the location of the tumor resection and the distance from the nipple-areolar complex to its new location. Once the tumor had been excised, 3 titanium clips were placed to identify the tumor bed during the planning of the radiation therapy. All patients in the study group were proposed symmetrization of the healthy breast using the same pattern. Lymph node staging was performed by sentinel lymph node biopsy in those patients with no clinical involvement of the axilla and by axillary lymphadenectomy in those with axillary involvement at diagnosis or metastatic involvement of the sentinel node. Axillary lymphadenectomy was performed in levels I/II, preserving the pedicle of the latissimus dorsi and the long thoracic nerve.
Adjuvant therapy. The patients with tumors that expressed hormone receptors underwent hormone therapy for 5 or 10 years, with tamoxifen for the premenopausal women and aromatase inhibitors for the postmenopausal women. Adjuvant chemotherapy was indicated according to the decision of our center’s tumor committee using the clinical guidelines corresponding to each period (8). The patients who required chemotherapy underwent, in most cases, a sequential regimen of 4 cycles of adriamycin and cyclophosphamide every 3 weeks followed by paclitaxel weekly for 12 cycles. Those patients with HER2 overexpression were prescribed trastuzumab to be taken every 3 weeks for 1 year.
All patients included in the study underwent tangential field breast radiation therapy at a 50-Gy dose in 25 fractions of 2 Gy each. In the event of tumor bed overprinting, we administered an additional 8–10-Gy dose, divided into 4 or 5 sessions. The women who underwent axillary radiation therapy and/or in the supraclavicular region were administered a 50-Gy dose in 25 sessions, to a depth of 3 cm. Axillary radiation therapy is indicated for women who have at least one of the following criteria: capsular rupture of the lymph node, lymphovascular invasion, grade 3 of the Scarff-Bloom-Richardson grading system, involvement of 3 or more lymph nodes and the absence of hormone receptor expression. The internal mammary chain was not irradiated in any case.
Neoadjuvant chemotherapy. Neoadjuvant chemotherapy was indicated for those patients with locally advanced tumors (stage III), poor breast-size-to-tumor ratio and subtypes of tumors with a high probability of full response to chemotherapy (triple negative, HER2 subtype). Those patients with HER2 overexpression were treated with dual anti-HER2 blockade (pertuzumab and trastuzumab).
Statistical analysis. All data were collected and analyzed using the SPSS program (SPSS v22; SPSS Inc., Chicago). We calculated the sample size assuming a confidence level of 95%, a statistical power of 85% and 10% loss, resulting in a total of 48 women needed for the study. The quantitative variables are listed as mean and standard deviation, and the qualitative variables are listed as numbers and percentages. The association between qualitative variables was compared with the chi-squared test or Fisher's exact test. After verifying the normality of the quantitative variables, we employed Student's t-test, ANOVA for independent groups, the Mann-Whitney U test and Kruskal-Wallis for dependent groups, as appropriate. To analyze the preoperative questionnaire, we calculated the percentiles for each domain and created a qualitative variable based on these percentiles, determining 3 satisfaction groups for each domain (low, medium and high satisfaction). Low satisfaction was defined as scores below the 25th percentile, medium satisfaction was defined as scores between the 25th and 75th percentile, and high satisfaction was defined as scores higher than the 75th percentile. We compared the baseline physical characteristics of these groups (weight, height, BMI, macromastia, menstrual state and age) and neoadjuvant therapy. With the patients who completed both questionnaires (preoperative and postoperative), we subsequently performed a comparative analysis to determine 3 groups of satisfaction/wellbeing: patients whose satisfaction worsened, patients whose satisfaction did not change and patients whose satisfaction and/or wellbeing improved. We determined the clinical characteristics that characterized each group and compared them using the corresponding statistical test.
Results
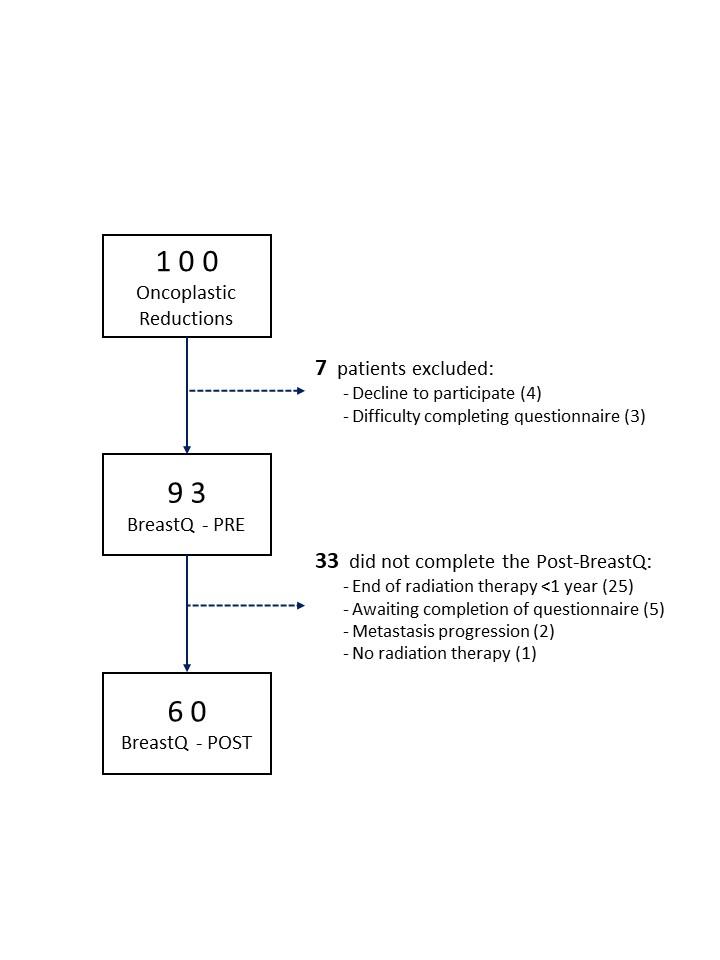
A total of 482 patients underwent surgery during the study period, and 104 were proposed OBR. We asked 100 patients with bilateral OBR to participate in the study after excluding 4 patients who underwent unilateral OBR. The preoperative questionnaire was not submitted to 7 patients (4 declined to participate in the study, and 3 had difficulties understanding the questionnaire). Ultimately, 93 patients covered the preoperative Breast-Q questionnaire (Figure 1). By the close of the study in June 2019, a total of 60 patients had completed the postoperative questionnaire, while 33 had still not completed it: 25 had not completed the year of breast radiation therapy, 2 presented progression to metastasis, 1 declined the breast irradiation and 5 were awaiting completion of the postoperative questionnaire once the year of breast radiation therapy had been reached.
Patient characteristics. The mean patient age was 50.2 years, and the mean BMI was 24.4 kg/m2.
Study of preoperative satisfaction and quality of life. During the preoperative assessment, there was lower satisfaction with the breast among the patients with macromastia and excess weight/obesity at the diagnosis, differences that were statistically significant. Furthermore, the preoperative questionnaire showed a poorer physical condition among the patients with macromastia. In contrast, we found no factors related to the psychosocial state and sexual wellbeing during the preoperative assessment.
Study of postoperative satisfaction and quality of life. The comparative study of the scores for the 60 patients who completed the preoperative and postoperative questionnaires showed a statistically significant increase in breast satisfaction and psychosocial wellbeing. Furthermore, there was an increase in physical and sexual wellbeing after OBR, but these differences were not significant. The patients with macromastia and those who underwent chemotherapy recorded a statistically significant increase in satisfaction with their breasts after OBR. The preoperative satisfaction with the breasts showed a relevant relationship with the final score, given that 73% of the women with low preoperative satisfaction improved their satisfaction, while 63% of the women with high preoperative satisfaction had poorer satisfaction. The study identified the women with macromastia as the only patient group who improved their physical condition after OBR (Table 4). In contrast, the study identified the women with antibody therapy as the factor related to worsening of the physical condition. The study showed an improvement in sexual wellbeing after OBR in the patients with macromastia. We found no factors related to variations in psychosocial wellbeing.
During the postoperative assessment, there was high satisfaction with the outcome, with the final result of the nipple-areolar complex and with the information received from the surgeon. Lastly, the postoperative questionnaire showed highest satisfaction in the assessment of the health professionals of the breast unit (surgeons, nurses and multidisciplinary team)
Follow-up. The mean patient follow-up was 31.1 ± 14.9 months. During the follow-up, 2 local relapses and 2 progressions to liver and lung metastases were detected (actuarial disease-free survival at 5 years, 89.3%; 95% CI 82.7–95.9%). One patient died due to liver metastasis at 8 months after the surgery (actuarial overall survival at 5 years, 98.9%; 95% CI 97.8–100%).